COSENTYX is covered as a 1st- or 2nd-line biologic in HS across Private insurance, Medicaid, and Medicare1*†
COSENTYX is included on most formularies for commercially insured patients1*
Resources to help you get patients started
on COSENTYX
Uninsured or underinsured patients will be connected to the Novartis Patient Assistance Foundation, Inc. to see if they are eligible for financial assistance.
*COSENTYX for subcutaneous is present on formularies as either a first-, second-, third-, fourth-, or fifth-line biologic. Actual coverage and reimbursement decisions are made by individual payers following the receipt of claims. Coverage information is subject to change by the relevant payer. Be sure to review the COSENTYX coverage criteria outlined by your patients' insurance providers.
†Certain payers have carve-outs that restrict utilization of manufacturer support programs.
‡The Covered Until You’re Covered Program is available for COSENTYX subcutaneous injection only. Eligible patients must have commercial insurance, a valid prescription for COSENTYX, and a denial of insurance coverage based on a prior authorization request. Program requires the submission of an appeal of the coverage denial within the first 90 days of enrollment in order to remain eligible. Program provides COSENTYX for free to eligible patients for up to two years, or until they receive insurance coverage approval, whichever occurs earlier. A valid prescription consistent with FDA-approved labeling is required. Program is not available to patients whose medications are reimbursed in whole or in part by Medicare, Medicaid, TRICARE, or any other federal or state program. Patients may be asked to reverify insurance coverage status during the course of the program. No purchase necessary. Program is not health insurance, nor is participation a guarantee of insurance coverage. Limitations may apply. Enrolled patients awaiting coverage for COSENTYX after two years may be eligible for a limited Program extension. Novartis Pharmaceuticals Corporation reserves the right to rescind, revoke, or amend this Program without notice.
§Limitations apply. Enrolled patients awaiting coverage for COSENTYX after 2 years may be eligible for a limited Program extension. Valid only for those with private insurance. Program provides up to $16,000 annually for the cost of COSENTYX and up to $150 per infusion (up to $1,950 annually) for the cost of administration. Co-pay support for infusion administration cost not available in Rhode Island or Massachusetts. Patient is responsible for any costs once limit is reached in a calendar year. Program not valid (i) under Medicare, Medicaid, TRICARE, VA, DoD, or any other federal or state healthcare program, (ii) where patient is not using insurance coverage at all, (iii) where the patient’s insurance plan reimburses for the entire cost of the drug, or (iv) where product is not covered by patient’s insurance. The value of this program is exclusively for the benefit of patients and is intended to be credited towards patient out-of-pocket obligations and maximums, including applicable co-payments, coinsurance, and deductibles. Program is not valid where prohibited by law. Patient may not seek reimbursement for the value received from this program from other parties, including any health insurance program or plan, flexible spending account, or healthcare savings account. Patient is responsible for complying with any applicable limitations and requirements of their health plan related to the use of the Program. Valid only in the US and Puerto Rico. This Program is not health insurance. Program may not be combined with any third-party rebate, coupon, or offer. Proof of purchase may be required. Novartis reserves the right to rescind, revoke, or amend the Program and discontinue support at any time without notice.
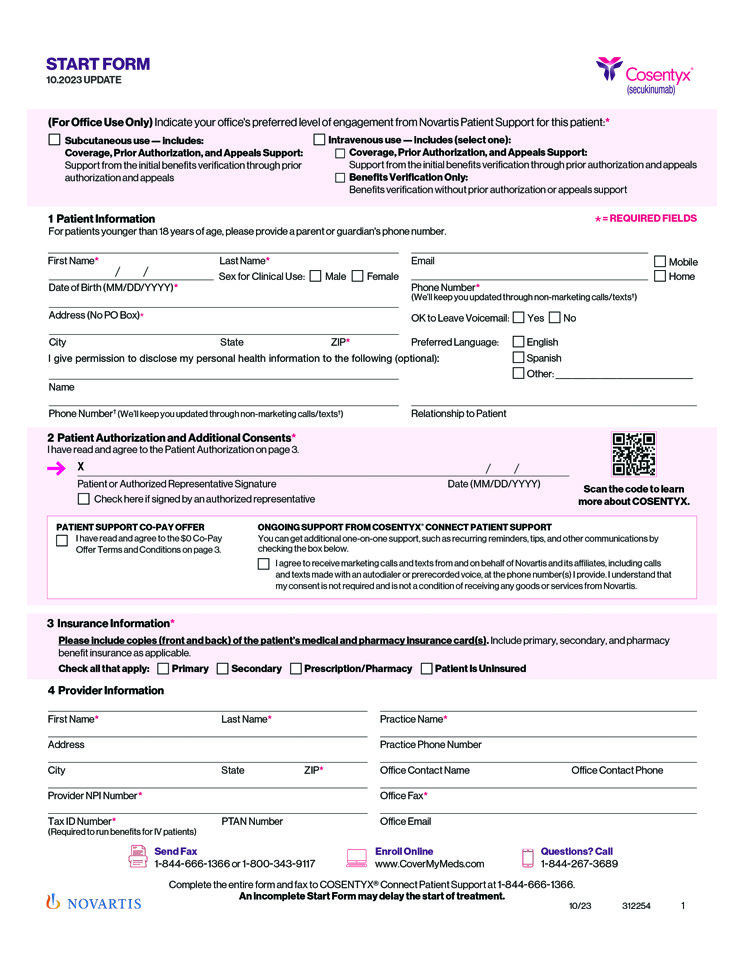
Start form
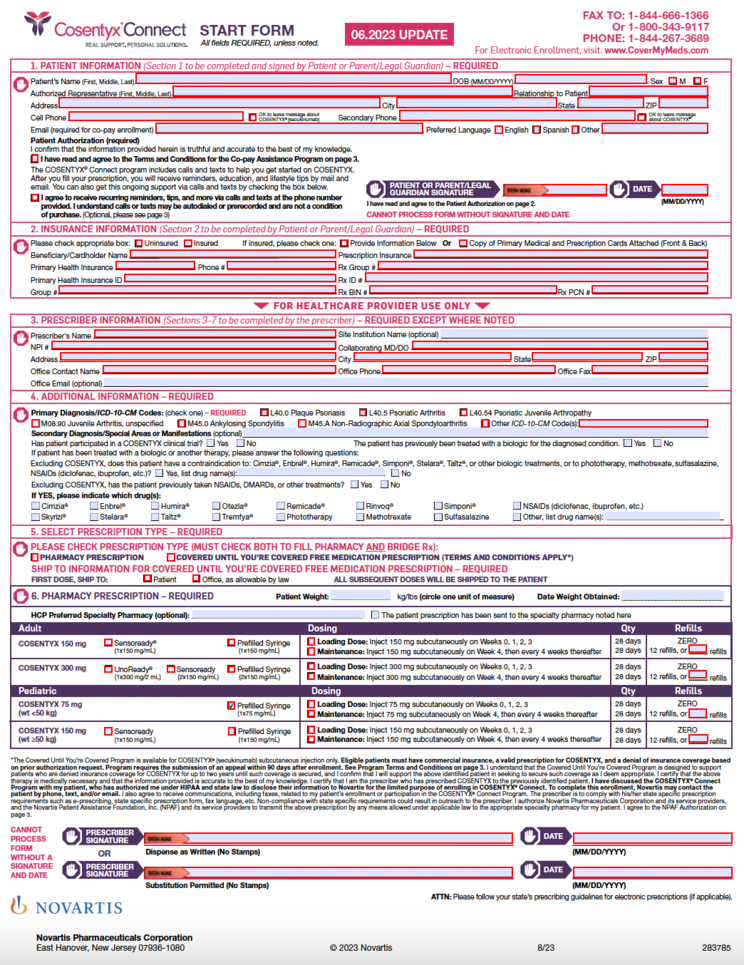
Spanish start form
